From stress to strength: The neuroscience behind burnout
Understanding how stress rewiring the brain can help leaders build healthier, calmer workplaces where people recover, grow and perform sustainably.
91% of UK adults reported high stress last year. Stress has become so normalised that exhaustion feels like the price of ambition. Chronic stress changes the way our brains function, eroding our capacity for focus, empathy and decision-making.
Burnout, says Sarah Noon, People Development and Training Manager at Change Mental Health, is a form of “biological wear and tear”, shaped by cultures that reward speed, availability and endurance over reflection and rest.
“We often talk about burnout as an HR problem or a culture issue,” Sarah explains. “But the truth is, it’s actually a brain health pandemic.”
In her work, she focuses on what neuroscience reveals about stress and how leaders can use that understanding to build workplaces where people perform sustainably rather than survive through strain. Sarah has seen how the science of stress can help us change how we work, lead and look after one another.
What happens in our brains – the stress triangle
The human brain uses three main regions to handle stress: the amygdala, the prefrontal cortex and the hippocampus.
The amygdala acts as an alarm system, detecting threats and activating the body’s fight-or-flight response. The prefrontal cortex manages reasoning, focus and emotional regulation. The hippocampus stores memory and learning, helping us find meaning in our experiences.
Under short-term, acute stress, this system works beautifully, sharpening attention and improving reaction time. But when pressure becomes constant and recovery never comes, the system starts to malfunction.
Long-term stress strengthens the brain’s alarm circuits and weakens the parts that help us stay calm and think clearly. Studies show that the amygdala becomes overactive, while the prefrontal cortex and hippocampus shrink in volume. In simple terms, our brains get stuck in ‘alert mode’.
Sarah recognises that pattern in her own journey. “Burnout forced me to slow down long enough to reflect and recognise that constant urgency was not a requirement. It was a habit,” she says.
When urgency becomes identity
Sarah’s own experience of burnout is similar to many you will find on the internet. Burnout didn’t just appear overnight. Raised in a working-class family, she learned early that work and worth were intertwined. Fast-paced, high-pressure environments felt natural. One day, the system she operated broke down.
It was that moment when chronic stress stopped being background noise and became impossible to hide.
“It was the wear and tear of my stress triangle. Years of chronic stress had rewired my brain to constantly anticipate more stress.”
Recovery began with noticing and recognising that the urgency she felt was the result of years of habit-building. Slowing down wasn’t about doing less but about doing things differently.
“I’ve learned to check in with my nervous system before I say yes,” she explains. “I ask myself, ‘Am I operating from purpose or from pressure?’ As a leader, I now try to model pace-setting that is sustainable. I encourage pause and recovery as part of performance, not something you earn after you’ve exhausted yourself.”
That shift changed how she supported others too.
“Someone on my team was struggling to deliver on a project,” Sarah recalls. “Before, I’d have jumped straight into fixing it or taken on the work myself. But I noticed the signs of a brain under pressure: short, clipped responses, perfectionism creeping in, overthinking every tiny detail. So, instead of pushing harder, I shifted the conversation from tasks to wellbeing and asked, ‘What’s feeling heavy right now?’”
By changing the tone, she found what was really going on: the person wasn’t lost or lazy, they were overwhelmed.
Her takeaway from this and many other situations is clear: when leaders stay grounded, the team follows. Calm spreads.
How workplaces keep the brain in threat mode
Even workplaces that mean well can trap people in a constant state of alert.
“Many habits are subtle and well-intentioned,” Sarah says. “Always-on communication, unclear priorities and unintentional celebration of speed over thinking time create unpredictability and a sense of never being ‘done’, which keeps the brain scanning for danger.”
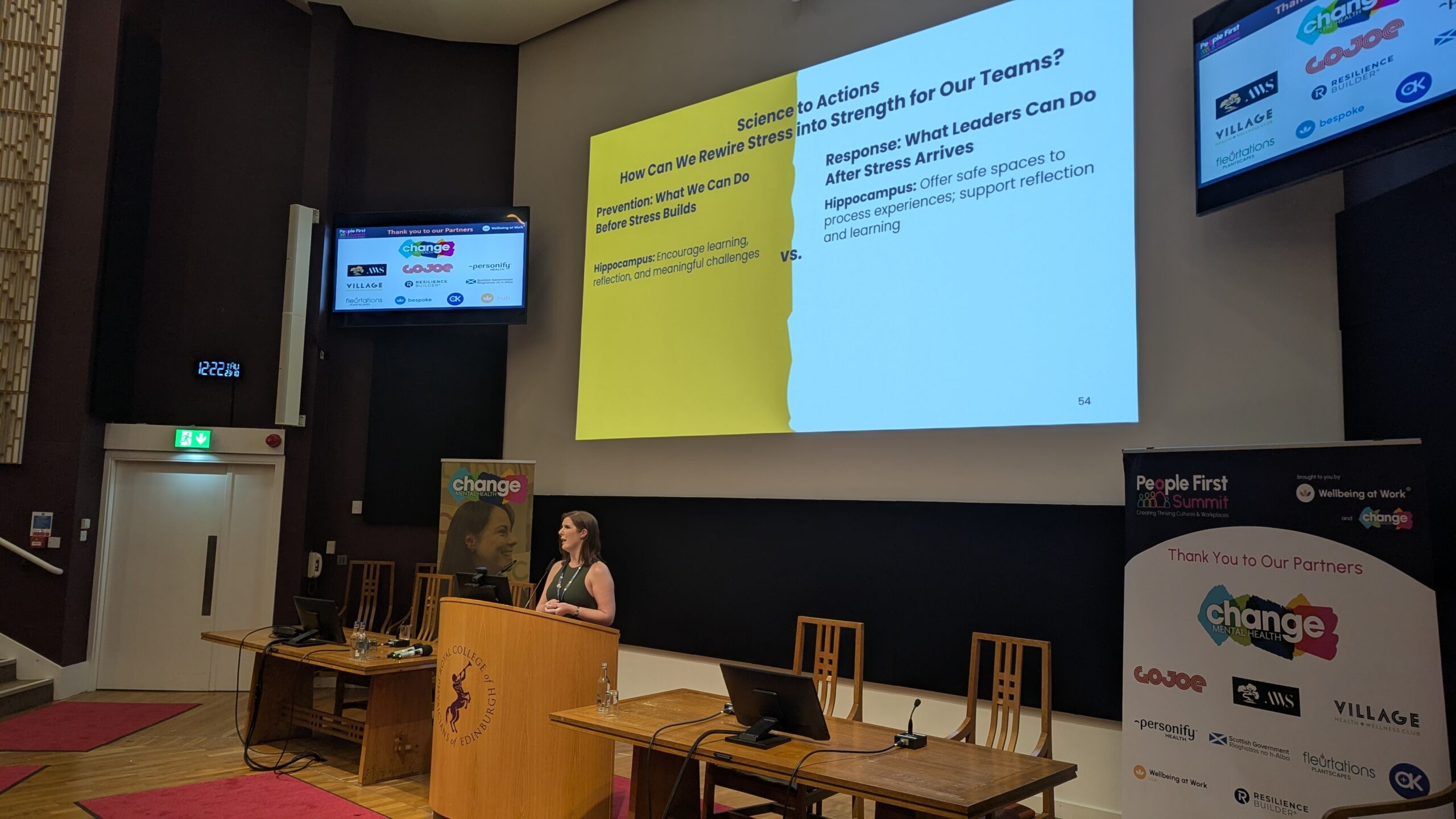
These constant micro-stresses teach the brain that work is unsafe. But the same systems that learn stress can learn calm. The antidote, she says, lies in small, deliberate shifts:
- Clear boundaries and expectations around response times.
- Transparency that removes ‘surprise’ tasks.
- Recognition of effort and recovery, not just output.
- Rhythms that include reflection alongside execution.
Predictable structures and fair workloads calm the amygdala. Time to think activates the hippocampus. Together, they rebuild the conditions for focus and creativity.
“Small shifts in how we work create big shifts in how safe people feel.
“Start meetings with context: ‘Why we’re here and what success looks like’, she suggests. “Build in breathing room, 50-minute instead of 1-hour meeting or optional cameras where possible. Avoid working during meetings. If you don’t have time to fully focus on a meeting, reschedule.”
Clarity is another simple but effective antidote.
“Say, ‘Here’s what I want to talk about and why.’ Default to positive intent and curiosity. That keeps the prefrontal cortex online.”
Predictable structure calms the nervous system. When staff know what’s expected and why, the brain’s threat response eases and thinking improves. Leaders who model calm communication give their teams permission to slow down, listen and contribute without fear.
“A regulated brain thinks better,” Sarah says. “This isn’t one of the soft skills to learn; it’s just smart.”
Building burnout recovery into culture
Almost one in three people employed in Scotland will quit their job because of its impact on mental health. Burnout doesn’t just vanish when someone changes jobs. Many of us arrive in new workplaces still carrying the impact of old environments. Sarah encourages leaders to start from a position of care.
“Operate from a place where you assume recovery is present, even if unspoken,” she advises. “When someone joins, make wellbeing part of onboarding.”
That can be as simple as asking what helps them do their best work, talking about energy rather than just task and signalling that pacing is valued.
“Make it OK to flag when something feels too stacked. Do it yourself. That’s leadership, not weakness.”
Recovery also needs to be visible at the organisational level.
“Model boundaries: if leaders don’t rest, no one else feels allowed to.
“Reward sustainable practices, not just heroic overtime. Make decompressing after big pushes expected, not exceptional. Talk openly about burnout as a shared system issue, not an individual flaw. Regularly ask, ‘What should we stop doing?’, to reduce cognitive load.”
Sarah Noon
People Development and Training Manager
Change Mental Health
These changes have an obvious effect of boosting morale, but they also change the biology of the workplace. Predictable routines calm the amygdala. Rest restores focus. Connection rebuilds the sense of safety that chronic stress erodes.
“Recovery takes reflection, rest and connection. When we get those right, people’s confidence and performance come back,” says Sarah.
Burnout reshapes the brain, but a culture that addresses stress and recovery reshapes the organisation. Healthy pace and high performance should not compete because they can exist in symbiosis, sustaining one another.
Sarah reminds us once more: “People shouldn’t be celebrated for surviving success. They should be supported in avoiding it.”
support
At Change Mental Health, this understanding is woven into the charity’s workplace training. The organisation helps employers build psychologically safe cultures through evidence-based courses on mental health awareness, stress management and compassionate communication. These sessions, designed and delivered by practitioners like Sarah, give teams the tools to recognise early signs of burnout, hold supportive conversations and make prevention part of everyday practice.
Find out more about our ready workplace mental health training sessions or get in touch to work with our team to create a bespoke training that fits your people, values and challenges.





